Advantages:
- Minimally invasive secretome therapy enhances Schlemm’s canal function, offering a non-surgical alternative to glaucoma treatment
- Secretome therapy promotes cellular repair and wound healing, addressing TM damage beyond Increased Intraocular Pressure (IOP) reduction
- Secretome therapy enhances aqueous outflow by upregulating tight junction proteins, offering a novel approach beyond conventional IOP-lowering drugs
- Dual secretome therapy synergistically balances proliferation and structural support, surpassing monotherapies like laser treatments or drugs
Summary:
Glaucoma, a leading cause of irreversible blindness, is primarily driven by elevated intraocular pressure due to resistance in the trabecular meshwork (TM) and Schlemm’s canal endothelial cells (SCE). Current treatments, which include topical medications, laser therapy, and surgical interventions, mainly aim to lower intraocular pressure but do not address the underlying cellular dysfunctions, leading to variable efficacy and potential side effects. This gap highlights the challenges associated with restoring normal tissue function and mechanical adaptability in the outflow pathway to achieve long-term disease management.
Our researcher introduces a novel cell-free therapeutic approach for glaucoma by administering a secretome derived from TM cells or their stem cells directly to SCEs.Secretome treatment, a rich array of cytokines, growth factors, RNAs, and proteins, enhances SCE viability, proliferation, wound healing, and reduced barrier function; all of which improve endothelial permeability and mechanical adaptability.
Furthermore, microarray and qPCR analyses identified potential biomarkers in TM and SCE cells, which are crucial for the proximal aqueous humor outflow pathway and play a significant role in glaucoma pathophysiology.
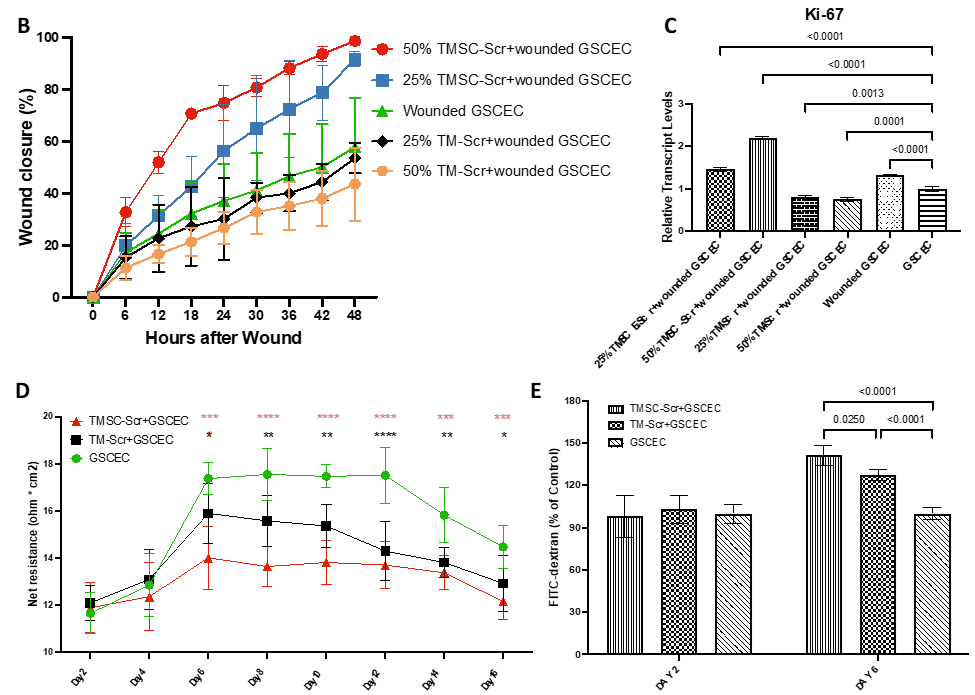
Effects of TMSC-Scr and TM-Scr on GSCEC Wound Healing, Proliferation, and Permeability. (B) Representative wound closure at 48 hrs with different treatments. Data are presented as mean ± SD. (C) Relative mRNA expression of Ki-67 in wounded GSCEC at 48 hrs with different treatments by qPCR. N=3. (D) TEER measures the permeability of GSCEC and GSCEC treated with 25% TMSC-Scr or 25% TM-Scr over 16 days. Data represent mean ± SD; n=6. Black stars compare TM-Scr and untreated GSCEC, while red stars compare TMSC-Scr and untreated GSCEC. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. (E) FITC-dextran permeability assays at days 2 and 6 post-treatment. Data are presented as mean ± SD; n=6.
Desired Partnerships:
- License
- Sponsored Research
- Co-Development